Introduction: Multiple Myeloma (MM) is the second most common hematologic malignancy in the US; over half of patients are ≥70y at diagnosis. Prior studies have shown that treatment preferences of older adults with cancer vary based on burden/intensity of current treatment and its impact on functional and cognitive well-being in addition to anticipated survival. However, no such studies exist among older adults with MM. We sought to understand health outcome preferences in a cohort of older adults with MM.
Methods: Using the Cancer and Aging Resilience Evaluation in Hematologic Malignancies Registry (NCT05556928), a single institution prospective observational study of older adults with hematologic malignancies undergoing systemic therapy, we identified patients diagnosed with multiple myeloma at age ≥50y who had undergone a geriatric assessment (GA) within 30 days of initiating a new line of therapy (1 st to 5 th line).Treatment preference was assessed using a 9-item health outcome preference attitude scale (Case et al Patient Educ Couns 2013), rating self-reported agreement with statements related to health outcomes on a Likert scale. Frailty was assessed using a deficit accumulation method as previously described (Giri S et al J Am Geriatr Soc 2023) We measured the proportion of patients reporting other outcomes being “as important” or “more important” than survival and compared the response between younger (<70y) and older (≥70y) adults. Subsequently, we built proportional odds models to study the factors associated with a greater prioritization of outcomes other than survival. All p values were two sided and the level of significance was chosen at 0.05.
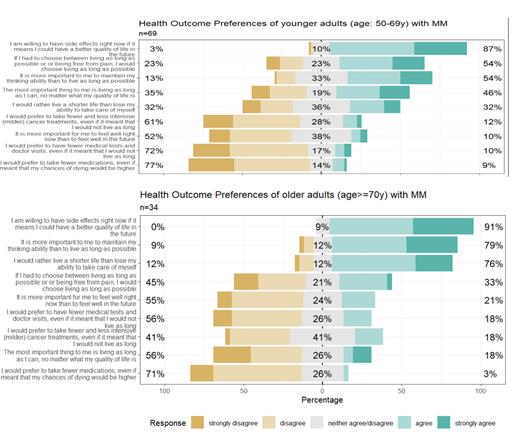
Results: Of the 228 patients initiating a new line of therapy between 01/2022 to 4/2023, 104 (47%) underwent treatment preference assessment. The median age at enrollment was 65y with 33% ≥70y; 62% were males, 57% whites; 19% had ISS stage 3 disease; 28% were frail on the CARE frailty index. In the younger (age <70y) vs older (age ≥70y) patients, 32% vs 77% agreed/strongly agreed with: “I would rather live a shorter life than lose my ability to take care of myself”; and 54% vs 79% agreed/strongly agreed with: “It is more important to me to maintain my thinking ability than to live as long as possible”. In multivariable models, age but not frailty, sex, race or disease stage were associated with health outcome prioritization other than survival. Each 1y increase in age was associated with and 8% (Odds Ratio 1.08; 95% CI 1.03-1.13; p value=0.001) and 4% (OR 1.04; 95% CI 1.0-1.09; p value=0.04) increased odds of rating functional independence and cognition respectively as more important than survival.
Conclusions: Three out of four older adults (age>70y) with MM rated other outcomes (particularly physical function and cognitive ability) as being more important than survival. Eliciting which outcomes are the most important for older patients can help define treatment goals and improve shared decision-making. Further, interventions focusing on preserving physical and cognitive function need to be tested in this population.
Disclosures
Bal:Astrazeneca: Consultancy; Janssen: Consultancy; MJH Lifesciences: Other: Educational content development ; Fate Therapeutics: Research Funding; Beigene: Research Funding; Amyloid Foundation: Research Funding; AbbVie: Consultancy; Adaptive Biotechnology: Consultancy; Bristol Myers Squibb: Consultancy. Costa:BMS: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Adaptive biotechnologies: Consultancy, Honoraria; Genentech: Research Funding; Pfizer: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal